Compounds Kill C. diff, Don’t Affect Other Gut Bacteria In Vitro

NC State researchers developed a drug-testing pipeline to help identify compounds that worked against the three stages of Clostridium difficile infection, and found that a compound that holds promise for treating antibiotic-resistant bacteria may also be able to control C. difficile infections by killing the harmful bacteria without affecting other bacteria in the gut.
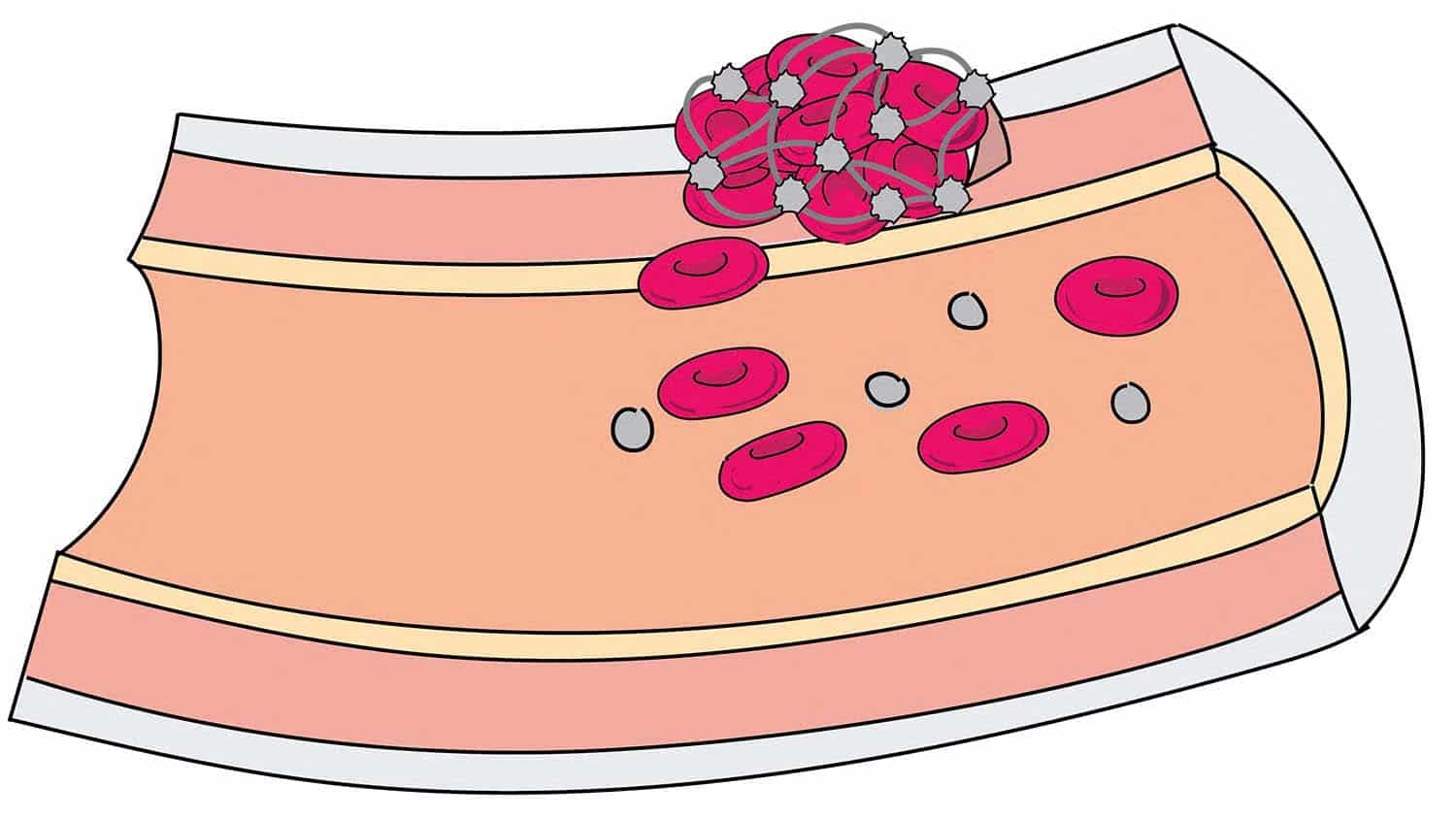
Clostridium difficile, or C. diff, is a bacterium that can cause painful and sometimes fatal infections: it is responsible for over 450,000 infections and 29,000 deaths annually in the United States. C. diff exists in the environment as a dormant spore. In a healthy gut other microbes within the gut keep C. diff in check. However, when the gut microbiota fail to keep C. diff in check; for example, when someone has taken antibiotics that kill off the “good” gut bacteria, the spores germinate, grow and produce toxins that damage the large intestine.
“The Catch-22 of C. diff is that the antibiotics that treat it exacerbate the problem by also eliminating bacteria that keep C. diff from growing,” says Casey Theriot, an assistant professor of infectious disease at NC State. “So when we look for compounds that can be effective against C. diff, we have to look at a number of factors, including the compound’s effect on the rest of gut microbiota.”
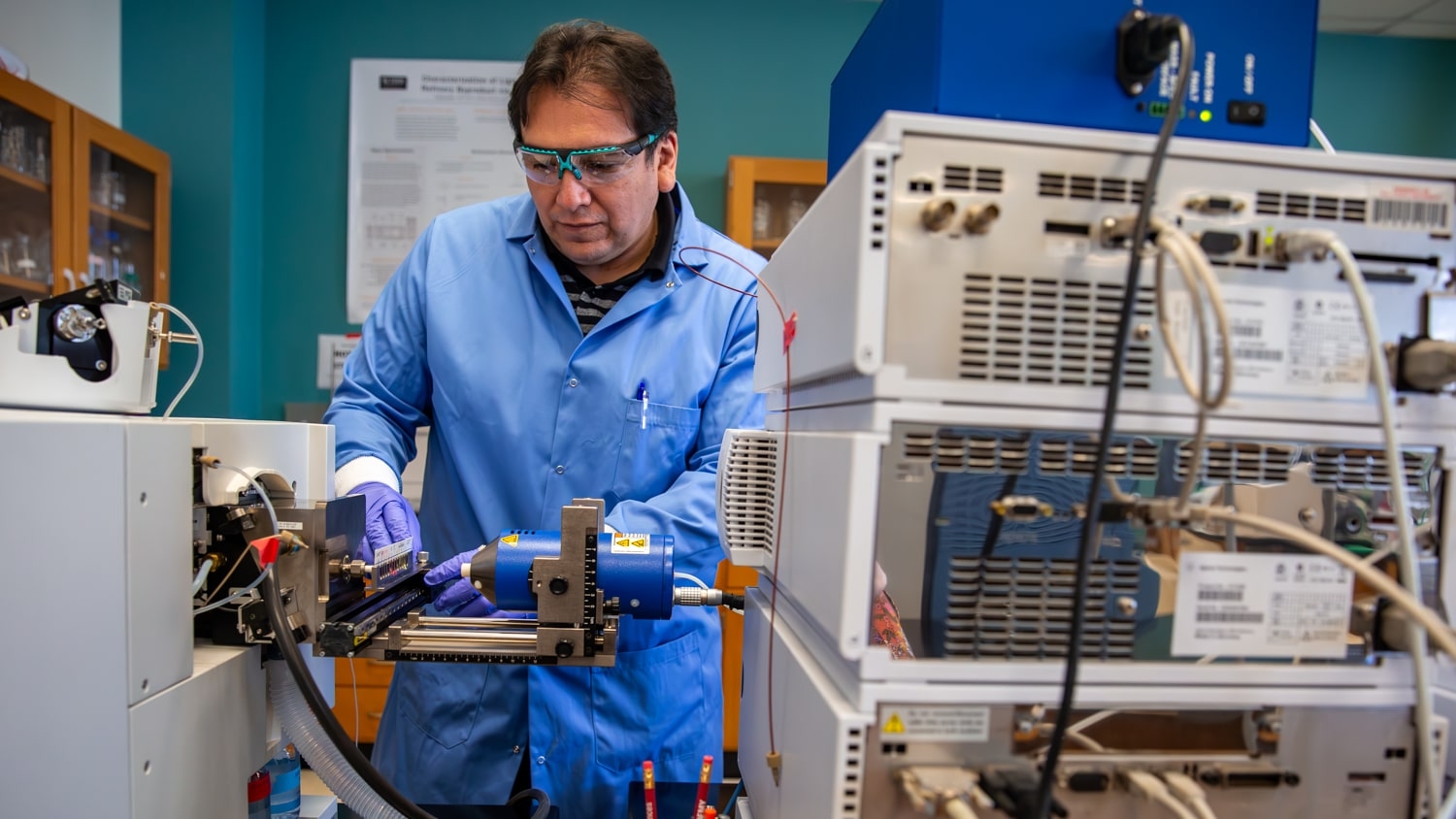
Theriot and her team, led by Rajani Thanissery, created a small molecule pipeline that addressed those factors to help researchers identify compounds that could be used against C. diff. The pipeline tested compounds against three different stages of the C. diff life cycle: growth, toxin production and sporulation, as well as against other gut bacteria. The goal was to screen and select compounds that could inhibit one or all of the steps in the C. diff life cycle.
One of the small molecules she tested – 2-aminoimidazole (2-AI) – gave her some surprising results. 2-AI was developed by former NC State professors John Cavanagh and Christian Melander. The compound, derived from sea sponges, is effective against antibiotic-resistant bacteria like MRSA. It works on these bacteria primarily by suppressing their ability to form biofilms or produce toxins, rather than killing the bacteria outright.
Thanissery screened eleven 2-AI molecules (compounds 1 through 11), provided by Daina Zeng and Raul Doyle at Agile Sciences, against C. diff in vitro. The molecules she screened were selected for their ability to inhibit C. diff growth, toxin activity and sporulation. Three molecules (compounds 1, 2, and 3) eliminated C. diff, but did not affect other bacteria. Compounds 4, 7, 9, and 11 inhibited toxin activity without affecting the growth of C. diff strains or the other microbiota.
“The results were both encouraging and surprising – we weren’t expecting the molecules to kill C. diff, since they primarily inhibit virulence factors,” Theriot says. “Our next steps will be to look more closely at the mechanisms by which 2-AI inhibits toxin activity.
“We were also pleased that our testing pipeline was able to successfully identify molecules that demonstrated activity against different aspects of C. diff infection. Hopefully other researchers can use our pipeline to screen future therapeutics in the lab before moving into preclinical animal models.”
The research appears in appears in Frontiers in Microbiology. Agile Sciences is a pharmaceutical company founded in 2007 by Melander and Cavanagh.
This post was originally published in NC State News.