Salmonella Loves Hydrogen Peroxide – And Helps Your Body Make More of it
Salmonella is a nasty little bacterium. The Centers for Disease Control and Prevention estimates that it sickens one in six Americans each year, with illnesses ranging from mild to fatal. Part of the reason that Salmonella is so effective in making us sick is that it is able to turn the body’s defense mechanism to its advantage. Now, new research from NC State describes just how Salmonella does what it does.
When the body detects a foreign bacterial invader, it recruits cells known as neutrophils. These specialized cells generate reactive oxygen species – simply put, they create hydrogen peroxide. In most cases, the hydrogen peroxide will kill the invading bacteria. But Salmonella is immune to the hydrogen peroxide. In fact, Salmonella can increase the amount of peroxide the neutrophils produce.
“Salmonella benefits from the presence of additional hydrogen peroxide because the peroxide kills the neighboring bacteria inside the intestine, removing competition for food and space to live,” says Johanna Elfenbein, assistant professor of equine medicine and co-corresponding author of a paper describing the work. “We already knew this exploit, but we wanted to understand how Salmonella induces peroxide production.”
Elfenbein, with graduate research assistant Trina Westerman and co-corresponding author Katie Sheats from NC State and colleagues from Texas A&M, did in vitro testing with donated human blood to see how Salmonella affects neutrophil peroxide production. They found that Salmonella’s flagellar motility – its ability to move to the intestinal cell wall – and something called the type-3 secretion system-1 (TTSS-1) work in concert to induce more peroxide.
“Essentially, TTSS-1 is like a needle bacteria make so they can inject proteins from inside themselves into a cell,” Westerman says. “Those proteins have targets that make the human cell behave the way they want it to. In Salmonella’s case, the proteins encourage the neutrophils to produce more peroxide.”
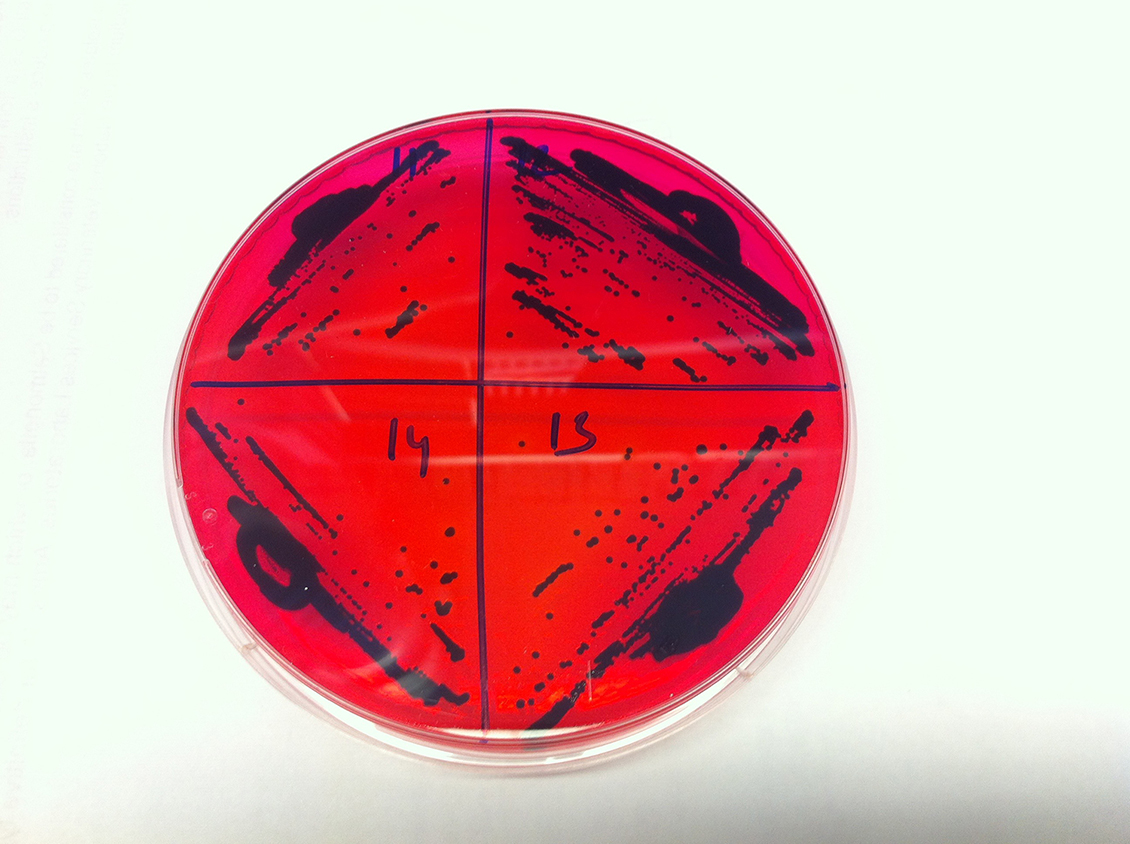
The researchers looked at peroxide production from neutrophils infected with the TTSS-1-wielding Salmonella Typhimurium (STm) – one of the two most common strains – and in neutrophils infected with a mutant Salmonella strain that lacks TTSS-1. They found a 1.5-fold increase in peroxide production from the neutrophils infected by the STm strain with the TTSS-1.
“TTSS-1 is already a well-described process,” Elfenbein says. “What we’re interested in is looking at the body’s response to infection, with an eye toward creating standard, infection-relevant methodology when studying this pathogen.
“This work shows the link between motility, TTSS-1 and increased peroxide production. Both of these processes are working together to influence how much hydrogen peroxide is produced.”
The research appears in PLOS ONE and is supported in part by the National Institutes of Health. Lydia Bogomolnaya, research assistant professor, and Helene Andrews-Polymenis, professor of microbial pathogenesis and immunology, both at Texas A&M, also contributed to the work.
This post was originally published in NC State News.


