Catalyzing Creative Concepts to Solve Commercial Challenges
The Chancellor’s Innovation Fund has selected six more research projects to support this coming year.

NC State University research helps turn today’s ideas into tomorrow’s solutions. That’s core to our land-grant mission. The Chancellor’s Innovation Fund (CIF), a competitive internal seed fund, has proven to be a powerful way we support that mission.
Chancellor Randy Woodson established the CIF in 2010 to help more NC State research bridge the gap between public and private funding — and ultimately turn into technology that both benefits consumers and addresses pressing problems.
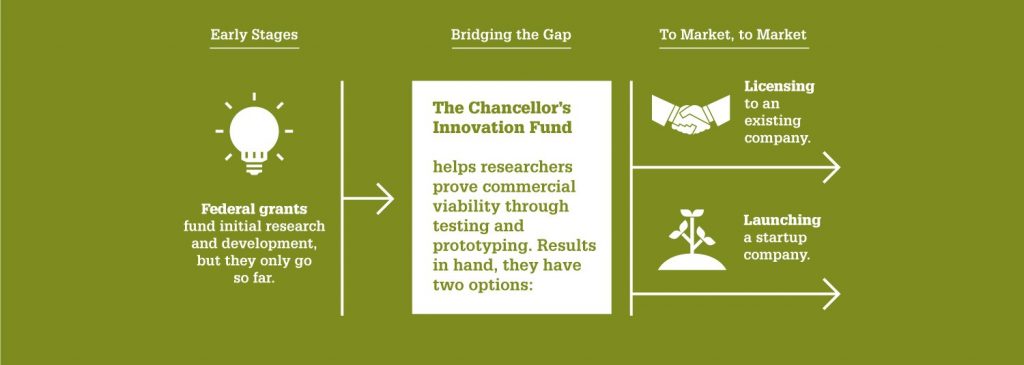
The CIF awards a select few of NC State’s best and brightest innovators tens of thousands each year to support short-term, commercially focused research projects. Over the course of the project — and for as long as needed afterward — awardees also receive help from the Office of Research Commercialization (ORC), which manages the CIF. ORC comprises business experts, intellectual property lawyers and others who can get researchers to start thinking more like startup founders — and make sure they’re in the right place and in touch with the right people at the right time.
Starting last year, thanks to the generosity of local entrepreneur Bill Spruill, researchers selected for CIF support also gain resources and counsel from Spruill’s 2ndF Research Commercialization Fund.
To date, 81 CIF projects have been awarded a total of $4.5 million. Past CIF winners have gone on to secure nearly $150 million in total funding since completing their respective projects. CIF projects have also led to the execution of 66 licensing agreements — which have generated $5 million in revenue for the university — and helped launch 37 NC State research-based startup companies.
This year’s winners are working on better ways to purify biologics; build non-toxic, non-flammable batteries; deliver cutting-edge cancer treatments directly to tumors; increase crop yield for corn farmers; protect hardware from hackers; and help surgeons repair heart valves.
To learn more about this year’s CIF research projects, continue reading.
Building Biocompatible Batteries

Batteries as we know them have never exactly been environmentally friendly. And today’s latest lithium batteries can fuel raging fires that bring billions of dollars worth of damage each year. Past attempts to invent greener, more sustainable batteries have all failed to yield voltages high enough for most practical applications.
But Amay Bandodkar, an assistant professor of electrical and computer engineering, believes he’s figured out how to pull it off. Bandodkar has developed a non-toxic battery made of environmentally benign materials. His biocompatible battery has a long shelf life; is non-flammable and lighter than lithium batteries; and can operate under extreme temperatures and pressures.
CIF and 2ndF support will be used to help demonstrate the batteries are comparable to commercial lithium batteries in price and performance, which will include manufacturing a pilot run with an industry partner.
Purifying Biomanufactured Therapies Faster

Purity, safety and efficacy are paramount for every pharmaceutical drug. But the purification process for modern-day biologics — gene therapies or vaccines powered by engineered proteins, antibodies and viruses — is complicated, lengthy and relatively inefficient. Biomanufacturing companies currently use a process called resin column chromatography to purify their products.
Longtime research partners Ruben Carbonell and Behnam Pourdeyhimi, in collaboration with Cristiana Boi and their colleagues Jinxin Fan and Joseph Lavole, have developed a new class of nonwoven membranes to replace resin columns and, in turn, speed up purification. They’ve shown their all-membrane process could cut processing time for antibodies by 70% or more. The membrane devices are designed to be disposed of after each use — eliminating the need to clean and sanitize the massive equipment found in plants today. The technology can be scaled up or down and is designed to work with all biologics.
Carbonell, the Frank Hawkins Kenan Distinguished Professor of Chemical and Biomolecular Engineering, and Pourdeyhimi, the William A. Klopman Distinguished Professor of Materials, and their team will use CIF and 2ndF support to make larger batches of membranes, many of which will be shared with potential industry partners to help accelerate adoption.
Fighting Food Insecurity
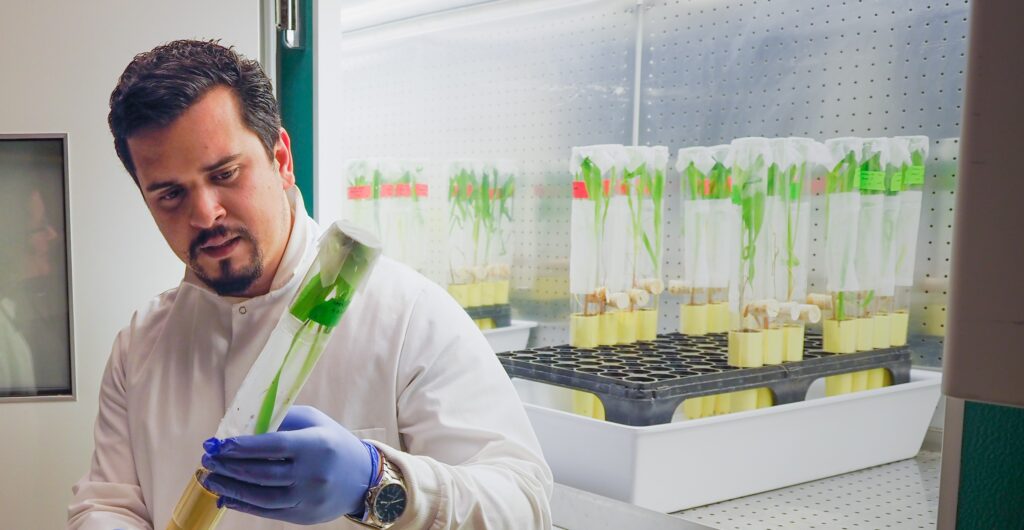
Humans have grown maize — commonly called corn — for nearly 9,000 years, and to this day, it’s still one of the most consumed crops worldwide. As global food insecurity continues rising steadily, Anna Whitfield knows corn production will remain crucial to feeding future generations. That’s why Whitfield, a Reynolds Distinguished Professor in the Department of Entomology and Plant Pathology and the director of the Emerging Plant Disease and Global Food Security faculty cluster, wants to make corn plants more disease-resistant and drought-tolerant.
How? By turning an old foe of farmers — maize mosaic virus — into their friend. Whitfield and two postdoctoral researchers, César Xavier and Deepjyoti Singh, have developed a brand-new viral vector — an engineered virus reprogrammed to carry genes into cells — that could make it faster and more efficient for crop science companies to deliver RNA to targeted genes of interest and ultimately to increase crop yields. She and her team’s MMV delivery system is designed to carry a much bigger payload than existing genetic modification tools can. Compared to other plant viruses, MMV can incorporate larger nucleic acid sequences.
Since addressing food security is the driving goal, the team will first and foremost concentrate on corn. But Whitfield says their rhabdovirus-based vector has the potential to work with other crops, too. Viral vectors already have a limited presence in agricultural biotech today, but their instability — or unpredictability — has hampered them. Whitfield hopes her team’s viral vector will prove to be more stable than previous, failed attempts others have tried to create for corn. If their MMV delivery system successfully meets safety standards, it would be the first FDA-approved viral vector for corn on the market.
The team will use CIF and 2ndF support to connect with potential partners and obtain the proof-of-concept data needed to commercialize the technology.
Protecting Hardware from Hackers
The average security breach costs organizations close to $4.5 million each, according to IBM. Meanwhile, it’s estimated that cybercrimes have increased 15% a year since the late 90s. And it’s not just software that’s susceptible to hackers and other bad actors. Hardware has inherent vulnerabilities, too.
Microarchitectural attacks exploit weaknesses in chip design. Prometheus, a platform invented by professor Samira Mirbagher Ajorpaz, is poised to become the latest line of defense against microarchitectural attacks. Powered by AI, Prometheus presents a tool chipmakers can use to identify vulnerabilities preemptively — prior to fabrication. Software development companies also stand to benefit, as Prometheus could enhance malware detection.
Ajorpaz will use CIF and 2ndF support to expand the functionality of Prometheus, as well as refine its user interface. Ajorpaz, an assistant professor of electrical and computer engineering, and her team will also work with potential customers and industry partners to develop targeted demos.
Delivering Immunotherapies Directly to Tumors
Many cancer patients now have more than merely chemotherapy to choose from to treat their tumors. Modern immunotherapies have revolutionized cancer treatment by programming a patient’s own immune system to target and destroy cancerous cells. As it stands, though, only about 25% of cancer patients successfully respond to immunotherapies. By and large, these groundbreaking therapies are currently delivered intravenously, which results in low retention rates for some tumors.
Instead of using an IV, researchers are looking for ways to inject cancer-killing drugs directly into tumors. David Zaharoff, an associate professor in the Joint Department of Biomedical Engineering, and his Ph.D. student Siena Mantooth have developed an injectable hydrogel that aims to maximize the amount of therapeutics that tumors retain. Their novel platform is designed to be adapted as needed — and could one day treat any type of solid cancer. Solid cancers account for nine out of every 10 diagnoses, which equates to 18 million cases annually.
Preliminary experimental data in mice shows that with their approach, a single injection of the hydrogel mixed with an immunotherapy can eliminate tumors and prevent the cancer from growing back.
CIF and 2ndF support will be used to connect with oncologists and assess the clinical feasibility of the hydrogel. Mantooth and Zaharoff still need to generate additional preclinical data on their platform’s safety and efficacy. If they receive approval to conduct large-animal trials later this year, though, it could get them through FDA review much faster.
Helping Heart Surgeons

If the heart’s mitral valve seal gets loose, blood can begin to leak or pump in the wrong direction. Severe blood leakage, called regurgitation, causes the heart to overwork — and can lead to heart failure. When leaks become severe, many patients opt for a surgically implanted ring or clip that reinforces the “annulus” around the valve, making backward blood flow much less likely. Medical advancements have made these procedures gradually less invasive, but for some patients, surgery is still too risky.
NC State University Faculty Scholar Joseph Tracy, a professor of materials science and engineering, might have found a way to make surgery a safer option for many more of the millions of Americans who have mitral valve regurgitation. Together with Dr. Muath Bishawi, a cardiac surgeon and clinical researcher at Duke University’s School of Medicine, Tracy and his now-former student Matt Clary, who recently earned his Ph.D. in materials science and engineering, have developed a magnetic device that could make it simpler for surgeons to anchor a metal ring around the mitral valve’s annulus.
A large part of open-heart surgery’s inherent risk stems from the need to temporarily stop a patient’s heart. The team’s device is designed to be implanted while the heart is actively beating.
With CIF and 2ndF support, the researchers will finish developing a functional prototype and also assess the FDA’s regulatory path to eventual clinical trials.


