NC State University has been awarded more than $1.3 million from the National Institutes of Health to study whether yeast can be used to discover new drugs faster, as well as aid existing antibiotics — and, ultimately, even help treat antibiotic-resistant infections.
The research project will be funded by an NIH Director’s New Innovator’s Award, part of the agency’s High-Risk, High-Reward Research program.
The research aims to determine if a type of yeast commonly used to brew beer or bake bread could also catalyze drug discovery for new kinds of antibiotics. Additionally, the researchers plan to engineer a probiotic yeast that could one day help doctors deliver antibacterial treatments more effectively.
“What we’re trying to do in this project is identify drugs that can stop the activity of the toxins bacteria make when they infect you,” says Nathan Crook, an assistant professor of chemical and biomolecular engineering at NC State, who will lead the research project.
Bacterial infections are often so painful, Crook says, because the bacteria behind them secrete toxic proteins — which damage our cells.
“They’ll start messing with our proteins inside our own cells, and that causes those cells to die or lose their structural integrity, thereby allowing the bacterium to further invade our tissues,” Crook says.
Every antibiotic available today works by indiscriminately destroying any bacteria it can find, including the “bad” bacteria responsible for the infection. And in some cases, like the gut microbiome, that means antibiotics end up killing lots of good bacteria along the way. When antibiotics kill that good gut bacteria, the body becomes susceptible to C. diff — an increasingly common antibiotic-resistant infection that can run rampant among hospital patients.
So researchers have long been looking for a way to neutralize the toxins that bad bacteria put out rather than eliminating the bacteria entirely. The hope is that a drug designed to target the toxins instead of the bacteria itself might allow doctors to treat antibiotic-resistant infections like C. diff much more effectively.
“The reason why this is a high-risk, high-reward project is because we haven’t found that drug yet,” Crook says.
Prior research has found potential candidates against the bacterial toxins behind C. diff, Crook says, but it “took several years of work by multiple labs” to figure it out.
“We wanted to know if there was a faster way to identify promising compounds,” Crook says. And he credits his graduate students with the “brain flash” to try using yeast.
“Yeast proteins are actually very similar to our proteins”
Using this High-Risk, High-Reward NIH funding, Crook and his research team primarily want to determine whether baker’s yeast can replace engineered human tissue cells in the preliminary tests conducted on chemical compounds that could be viable candidates for new antibiotics.
“Yeast proteins are actually very similar to our proteins,” Crook says. “And in some cases, the targets of the bacterial toxins present in our own cells — the things they’re trying to mess up – are also present in yeast.”
Thanks to these similarities, Crook and his team think yeast might make the perfect test subjects for treatments that seek to stop bacterial toxins from wreaking havoc on their host’s cells.
“By putting these toxins on yeast, we were able to kill the yeast — and that sounds like a bad thing, but for us, it was actually a good thing,” Crook says. After introducing the toxins to yeast cells, Crook says you could then create control and treatment groups to quickly test the efficacy of certain promising compounds.
Part of the reason drug discovery can take so long is that it’s painstaking and time-intensive to culture human cells “or even a tissue-like system.”
“You can only do a couple of those at a time. But with yeast, you can grow millions of them at once,” Crooks says.
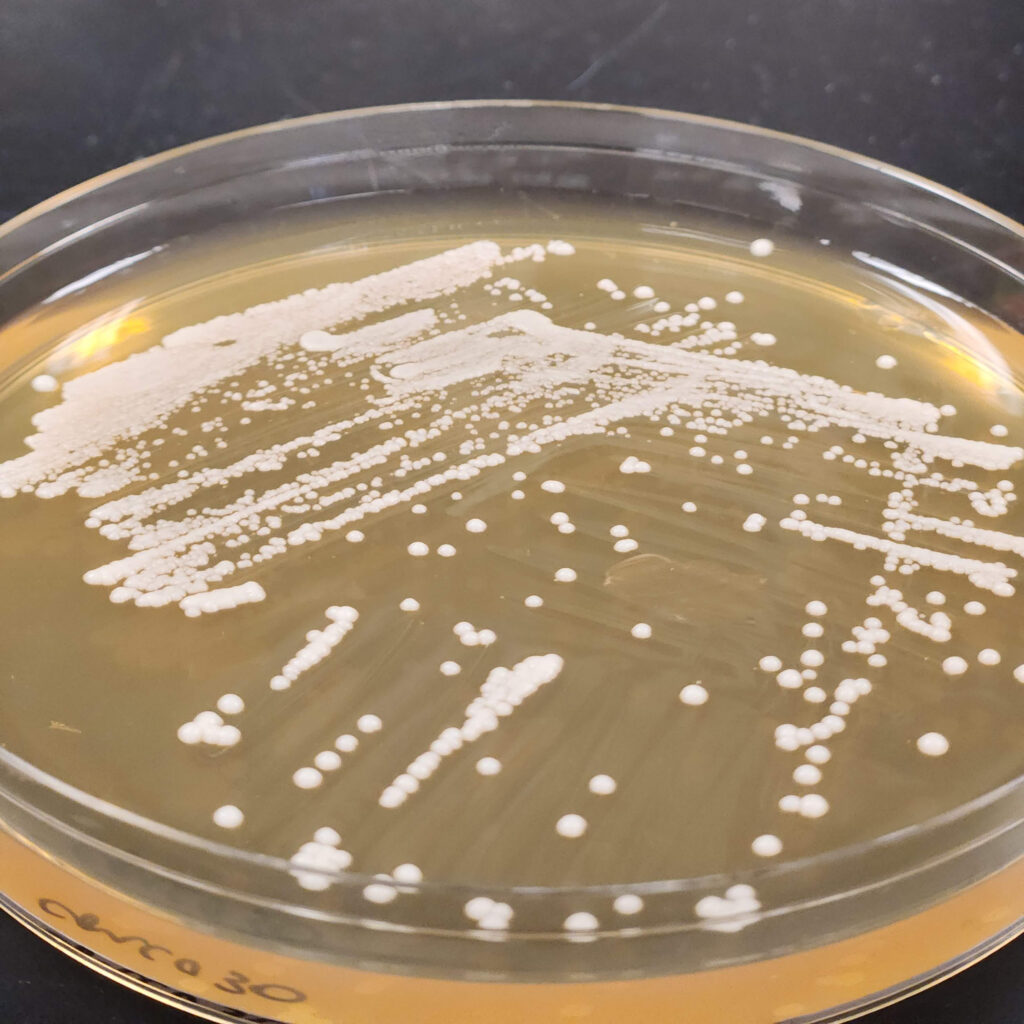
So if yeast can serve as a viable substitute for human cells, it could one day dramatically speed up the early experiments that kick off drug discovery and development.
Crook says that this work will initially focus on screening potential C. diff treatment candidates, but that if successful, the outcomes could be applied to techniques for identifying viable treatments for other types of antibiotic-resistant infections and perhaps, more broadly, to drug discovery and development in general.
The NIH Director’s New Innovator’s Award was established in 2007 to support “highly innovative” work led by researchers early in their careers. These awards support “exceptionally creative early-career investigators who propose innovative, high-impact projects in the biomedical, behavioral or social sciences…,” according to the NIH.
- Categories: