Powering Breakthroughs at the NC State College of Veterinary Medicine
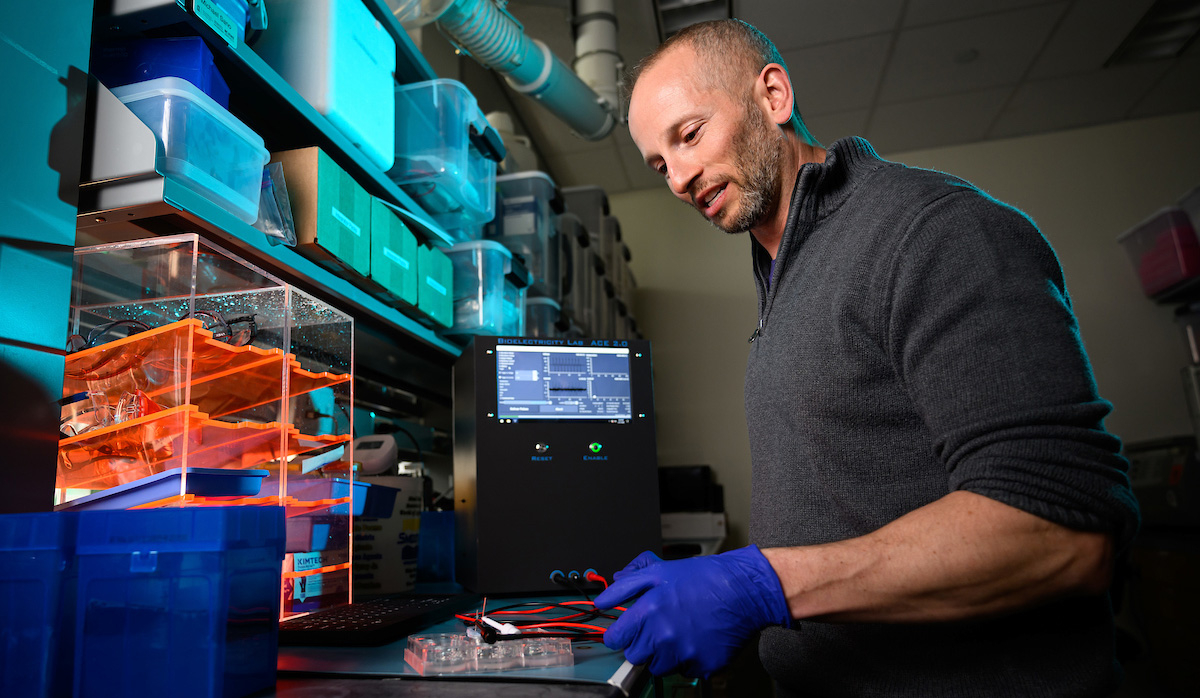
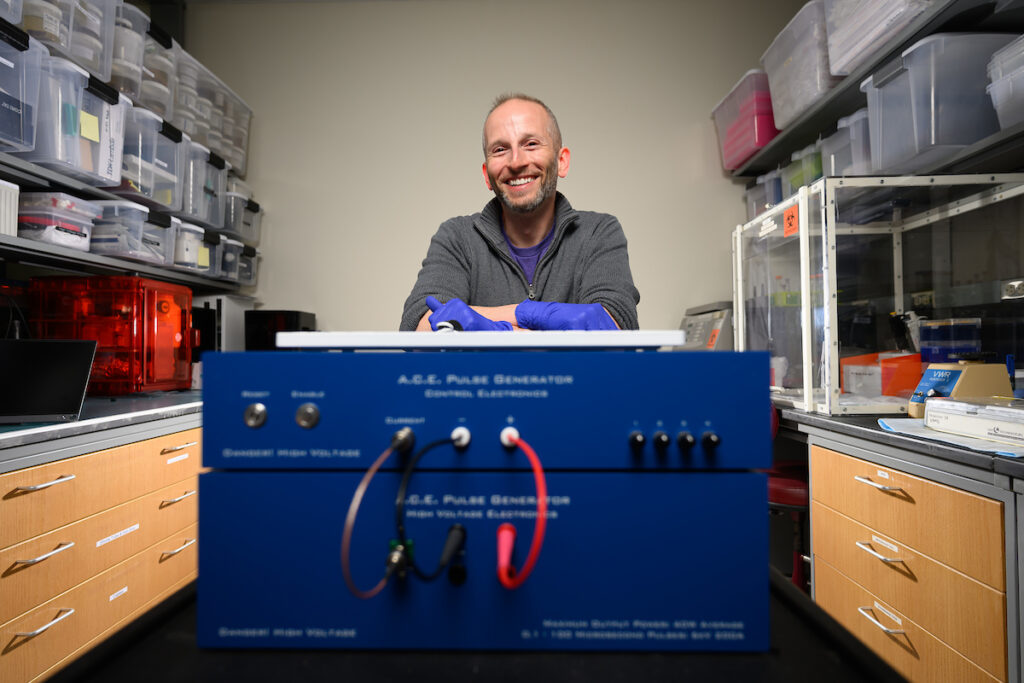
Electricity will soon be doing more in health care than just powering machines. With the research of Dr. Mike Sano and the bioelectricity lab at the NC State College of Veterinary Medicine, it could be the key ingredient in groundbreaking medical advancements from vaccines to cancer therapies.
“Everything in our body has an electric component,” Sano said. “We have a lot of signaling that happens through electricity, and there are a lot of bioelectric phenomena that are governed by electricity, especially on a small scale. It turns out that super interesting phenomena arise when you apply external fields to these already electrically reactive materials.”
In his search for a new cancer treatment for animals and humans, the associate professor is currently harnessing the power of electricity to target and destroy inoperable tumors. In recent clinical trials with client horses, the therapy eliminated 80% of tumors when used at the highest level.
“Technologies like this are so good that you don’t need to go through six months of chemotherapy and lose your hair and have your fingernails fall off,” Sano said. “The goal is to replace those really harsh therapies that have middling effectiveness with something that is much more effective and has fewer side effects.”
And that’s just one way bioelectricity could be changing health care.
Harnessing Bioelectricity
Sano’s vision for using electricity in medical treatments built slowly throughout his education. He studied electrical engineering and mathematics at the University of Buffalo as an undergraduate but was introduced to the capabilities of bioelectricity during his doctoral work at Virginia Tech.
“I was hooked immediately,” he said. “This combination of engineering, electronics and biology was fascinating.”
His doctoral research transitioned from studying bioprosthetics to using high-frequency electric fields to isolate and identify cancer cells in blood samples based on cells’ electric properties. As he worked to determine the maximum amount of electricity he could apply to isolate a cell for the diagnostic, Sano also learned at what point the electricity killed the cells he was trying to examine.
“I was really good at figuring out where that threshold was,” Sano said. “Through the process, I got a good understanding of the biophysics of what was happening.”
His short — at a nanosecond-level — but powerful electrical pulses were making the molecules in cells move rapidly and farther apart, eventually causing the cell membrane to develop pores. Once pushed far enough, those holes in the cell membrane ruptured, killing the cell. Nanosecond pulses also allowed for more voltage to be applied to cells without creating so much heat that the electricity would damage other tissue, blood vessels or nerves nearby, making it a viable approach to use in living things.
His Ph.D. adviser was already working on using bioelectricity to treat cancer, and with the discovery of Sano’s faster, shorter electric pulses leading to cell death, a new approach to cancer therapy started to develop. The goal: create a simplified device that could treat tumors ranging in size from a quarter to a golf ball in what are typically inoperable locations of the body.
Sano continued developing the therapy as a postdoc at Stanford University and brought it with him in 2017 when he became an assistant professor in the NC State-UNC Joint Department of Biomedical Engineering. Six years later, he joined the College of Veterinary Medicine to continue to develop the therapy — now called Integrated Time Nanosecond Pulse Irreversible Electroporation, or INSPIRE.
Changing How Cancer is Treated
Intent on translating the novel cancer therapy to a clinical setting, Sano immediately began looking for a veterinary partner in Raleigh and found Dr. Callie Fogle, a clinical professor at the CVM who works with horses at the Large Animal Hospital.
Fogle had experience with electrochemotherapy machines, which use principles similar to Sano’s INSPIRE but have one significant difference: The horse has to be anesthetized, or laid down, for the procedure.
“He was able to manipulate the electrical current in such a way that we could treat standing horses,” Fogle said. “With the electrochemotherapy machine, you could only treat anesthetized horses because the muscle contraction was very strong. To be able to provide that in a standing horse decreases the risk for the horse and the expense.”
Before an INSPIRE treatment, Sano and his team run a scan of a tumor through a computational model that determines where to place electrodes and how much voltage to use. The procedure, which delivers electrical pulses directly to the tumor, lasts between three and five minutes.
Sano and Fogle began a clinical trial using INSPIRE in 2022 to treat equine cancer patients with melanoma, examining how different voltages and speeds of the electrical pulses impacted tumors.



The results were promising.
The results also showed that the therapy packs a powerful one-two punch for cancer treatment. When the electricity kills the tumor, enough biological information is left behind that the immune system will recognize and attack the disease if it occurs elsewhere.
“We’re not just killing the tumor, but we’re killing it in the right way for the immune system to come in and recognize the tumor as something dangerous and start to mount an attack against it,” Sano said. “By the time most tumors reach the size of a golf ball, they’ve started to metastasize. It’s not enough to just kill that tumor. You really need to help the body respond to that disease that is now spreading around the body.”
The treatment has already altered the landscape for clinical cancer treatment at the NC State Veterinary Hospital.
“INSPIRE has allowed us to perform more advanced tumor treatment without a really large price tag or asking owners to ship halfway across the country to a facility that has a linear accelerator or radiation,” Fogle said. “It has already changed the way we treat tumors here, and I think we see horses from outside our normal referral radius because of this therapy.”
INSPIRE has now been used with more than 100 horses at NC State, and Sano has been able to work with other CVM veterinarians to expand clinical trials into dogs with liver and breast cancer — seeing more positive results there.
With promising signs, Sano said, INSPIRE could provide a new approach to treating cancer in humans when radiation and chemotherapy can’t hit the mark and surgery isn’t an option.
“We can burn it out, but if it’s near a blood vessel, like most tumors are, then you can’t burn it out. You could try and freeze it, but again, if it’s near a major blood vessel or a critical nerve, you can’t do that,” Sano said. “The reason why INSPIRE is needed is because other therapies fall flat.”


A New Approach to Vaccines
While cranking up the power to kill a cell is the principle behind INSPIRE, Sano is also looking at how the same concept can be used — turned down a few notches — to push cell membranes to the brink without rupturing. Creating holes in the membrane that then reseal themselves may be the key to making DNA vaccines a reality.
Similar to the mRNA vaccines developed to address the COVID-19 pandemic in 2020, DNA vaccines allow scientists to go from pathogen to a vaccine candidate rapidly. Unlike mRNA vaccines, which require constant refrigeration, DNA vaccines are shelf stable. During the pandemic, cold storage became a critical obstacle in the supply chain of the new vaccine.
“You can take a DNA vaccine, put it in your backpack and march across the desert, no problem,” Sano said.
But the need for cold storage is by design: An mRNA vaccine causes the body to make a specific protein to protect it from a virus, but it degrades quickly to prevent the body from making too many proteins. DNA vaccines, though better for storage, won’t enter cells on their own. They need an extra jolt in the form of a nanosecond electrical pulse that opens cell membranes and allows the vaccine in.
“We need to give it a push, and the way we do that is with electricity,” Sano said. “We use electric pulses that push the DNA into the cell to improve the efficacy of those vaccines. We just started working on it during the pandemic. We have shown it works in a dish, and now we’re trying to scale up.”
Eventually, that vaccination process could look as simple as a device, like a noncontact thermometer, delivering the vaccine and electric pulse simultaneously without the patient feeling anything. It would make current vaccinations more convenient and efficient and even open the door to even more impressive treatments.
“There’s a number of cancer vaccine candidates out there, and there’s also big agriculture applications — avian flu, for example, things where you need to vaccinate really big populations, but you can’t do it in this clinical setting,” Sano said.
Sano said the ability to harness electricity into a health care tool in these ways has progressed rapidly over the last decade, and there are no signs of the work slowing down. It’s just a matter of getting the equipment from the lab bench to patients. It’s a task he is up for.
“I have a very clinically focused mentality,” he said. “My goal is to get these technologies into the clinic and to patients.”
This post was originally published in Veterinary Medicine News.